
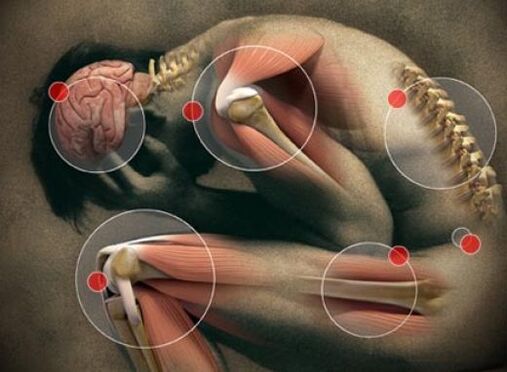
Joint pain- These are unpleasant sensations of pain, pulling in the joint area, the intensity of which sometimes reaches the level of pain. The symptom is combined with muscle pain, weakness, weakness, tingling, limited movement and may precede joint pain (arthralgia). Joint pain is associated with lesions of the musculoskeletal system, infections, diseases of the hematopoietic system and vascular pathology. To identify the cause of the disorder, laboratory tests, ultrasound, radiographic and invasive methods are used. Treatment includes treating the disease that caused the pain.
Causes of joint pain
Mild or moderate joint discomfort is not always a manifestation of a pathological process. Sometimes the symptoms have natural causes. Transient joint pain is felt when wearing uncomfortable shoes, and in people sensitive to the weather - when the weather changes. During puberty, pain in the shoulder and knee joints is caused by insufficient blood supply due to accelerated bone growth.
Significant physical activity
During intense training or heavy work, a common cause of the symptom is overloading of the musculo-ligamentous apparatus, less often it is caused by microtraumas of the cartilage and synovium. A typical combination of joint pain and bone and muscle discomfort. Discomfort in the joints and muscles occurs immediately after the impact of physical activity or against the background of prolonged monotonous work with constant tension in the same muscle groups. Joint pain occurs without fever. With large overloads, a moderate violation of the general condition and weakness is possible.
The disorder can last up to several days and, with limited physical activity, gradually decreases until it disappears completely without any treatment. If pain caused by sports or heavy physical work is replaced by constant pain, swelling in the wrist, elbow, shoulder, ankle, knee and hip, as well as limitation of usual movements, you should visit a doctor.
Age-related changes in the musculoskeletal system
The causes of moderate bone and joint pain in the elderly are degenerative processes with loss of calcium, thinning of the bone bundles, damage to the blood supply of the cartilage and a decrease in the volume of intra-articular fluid. Mild discomfort is only the first manifestation of senile joint damage. Typically, periodic disturbance occurs after 45-50 years. At the age of 60-65, an unpleasant pain appears even with little effort, accompanied by stiffness of movement, bending, change of gait and gradually gives way to pain.
pregnant
Complaints about joint pain are made more often in the second half of pregnancy. Pulling discomfort and pain is usually felt in the joints of the pelvis and lower extremities. It intensifies at the end of the day, after prolonged standing or walking long distances. A night's rest eases the condition. Joint pain during pregnancy is caused by the following reasons:
- Lack of vitamins and minerals. The biggest role is played by the lack of calcium and vitamin D, leading to osteomalacia. A feature of the symptom manifestation is a feeling of pain not only in the joints, but also in the bones, fatigue, the presence of other signs of hypocalcemia and hypovitaminosis D - caries, brittle nails, muscle weakness, muscle pain and frequentand ARVI.
- Significant weight gain. Joint discomfort is more often a concern for pregnant women who gain a lot of weight or those who are obese. Pains at the end, and eventually in the middle of the day, are felt in the hip joints, knees, ankles, whose cartilages experience loads several times higher than allowed. To alleviate the condition, women deliberately limit physical activity, which leads to even faster weight gain.
- Softening of cartilage and ligaments. About half of pregnant women experience discomfort in the pelvic joints caused by the action of the hormone relaxin. In most cases, the concern is in the nature of pain in the pubic area and hip joints. In a pathological course with the development of symphysitis, painful sensations are replaced by pain, which intensifies when pressing on the uterus, trying to separate the legs, during sex. The appearance of pain in the pubic area is a serious reason for a visit to the obstetrician-gynecologist.
- Carpal tunnel syndrome. A specific manifestation found in the 2-3 trimester in almost 20% of pregnant women is the so-called tunnel syndrome. The cause of the disorder is swelling of the soft tissues of the hands and compression in the carpal tunnel of the nerves that pass to the fingers. In addition to excruciating pain in the small joints of the hand, patients complain of skin numbness, tingling and crawling sensations. The condition improves with an elevated position of the arms.
Obesity
In overweight people, the pressure on the cartilage tissue increases, causing it to wear out faster. The degenerative-dystrophic process usually involves large joints of the lower extremities and intervertebral joints. The disorder increases with the progression of obesity. Discomfort in the joints first manifests itself in the form of pain without fever until the end of the day, then the increasing destruction of cartilage leads to the development of deforming arthrosis, spondylosis, osteochondrosis with a sharp pain syndrome that limits the patient's motor activity.
Acute infections
Body and joint pains are one of the early (prodromal) signs of many acute respiratory viral infections. The main causes of joint discomfort are intoxication of the body due to the spread of viruses and bacteria, the accumulation of toxins and the development of the inflammatory process. Usually the patient complains that the whole body hurts, there are mild and moderate pains in the joints as well as in the muscles and bones. The symptom is accompanied by weakness, fatigue, insomnia and frequent awakenings. Simultaneously with signs of pain and general ill-treatment, chills and hyperthermia are observed.
The most pronounced pains in the joints and body are with the flu. Up to 50% of patients experience constant pain in the legs, arms and torso. The intensity of the pain is so high that it becomes difficult for a person to perform the simplest actions - get out of bed, go to another room, get a glass of water. The situation is aggravated by high temperature (febrile) and severe headaches. Sore throat and nasal congestion occur after a few hours or even days. Less joint discomfort occurs with parainfluenza, an adenoviral infection.
A feeling of pain in the joints is possible with acute infectious lesions of the gastrointestinal tract - toxic food infections, salmonellosis. Painful joint pains of varying intensity appear suddenly a few hours after consuming contaminated food and are combined with a sharp increase in temperature, severe chills and headache. Pain is preceded by nausea, vomiting, pain in the abdominal cavity, foul-smelling diarrhea with mucous impurities and sometimes blood.
Collagenoses
Joint pain is a harbinger of most diseases that occur with autoimmune inflammation of connective tissue, including joint tissue. Localization, prevalence and intensity of unpleasant sensations are determined by the characteristics of a particular collagenosis. The general patterns are the involvement of certain groups of joints in the process, a gradual increase in sensations up to excruciating debilitating pain, observed first during movements and then at rest. Deformation of the articular joints is possible. The main systemic inflammatory causes of the disorder:
- Rheumatism. The symptom is "unstable": aching pains and then pain are felt on the other hand in the large joints of the arms and legs - elbows, shoulders, hips, knees, ankles. The affected areas are swollen. Joint discomfort is often preceded by a sore throat. With treatment, joint changes are reversible.
- Rheumatoid arthritis. Unpleasant sensations often appear after 40 years. A typical feeling of pain in the small joints of the hands and feet, combined with noticeable swelling and stiffness in the morning. In the future, pain and curvature of the articular joints come to the fore.
- Systemic scleroderma. It is characterized by variable localization of pain sensations, the presence of stiffness in the morning in the joints of the hands, elbows and knees. Aches and pains are usually symmetrical. The swelling is short-lived. Due to the sclerosis of the skin, the mobility of the articular joints is limited, damage to the tendons causes a feeling of friction during movement.
Osteoarthritis
The pain syndrome in the initial stages of the disease is mild and is perceived as discomfort, pain in the joints of the legs and less often in the arms. The immediate cause of osteoarthritis is the degeneration and destruction of cartilage tissue. Typically, sensations of pulling or pain without fever appear in adulthood and old age. Pain may start earlier in the presence of occupational hazards (vibration, heavy physical work). Gradually, the joints become stiff, the person experiences severe pain and difficulty in walking and taking care of himself.
Metabolic disorders
The causes of metabolic disorders in which joint pain occurs are insufficient supply of vitamins, minerals, accelerated accumulation or excessive secretion of metabolic products. Unpleasant sensations are caused by inflammatory or dystrophic processes, have different severity and most often serve as a manifestation of pathological conditions such as:
- Osteoporosis. When calcium is washed out of the bone tissue, the articular surfaces of the bones become fragile, the cartilage becomes thinner, which is accompanied by a feeling of pain. The pain syndrome gradually increases from mild pain to severe arthralgia, combined with unpleasant sensations in the bones and muscle weakness. The joints that experience the maximum load are most often affected - hips and knees; the shoulder, elbow and ankle are less commonly affected.
- gout. A slight pain in the big toe is already a concern in the preclinical stages of the gout process. There may be unpleasant pain in the knees, elbows, wrists and fingers. Accumulation of urates in the joint cavity leads to a rapid manifestation of the disease with a change from pain to acute painful joint pain that does not subside for several hours. The affected joint is hot to the touch. There is redness of the skin and limited movement.
Oncological diseases
In acute and chronic leukemia, widespread osteoarticular pains, followed by pain, often occur even before obvious pathological changes in a general blood test and other clinical symptoms - general malaise, night sweats, fever, loss of appetite, bleeding. Unpleasant sensations at first hurt periodically, then constantly strong, weakening the patient.
Hodgkin's lymphoma and lymphogranulomatosis are characterized by a combination of joint pain with muscle discomfort, weakness, enlargement of lymph nodes and other lymphoid formations. Pain sensations are common, usually moderate. A short period of pain in the knee joint and thigh muscles, which intensifies at night and with exertion turns into constantly increasing pain with lameness, is observed with osteosarcoma. Other nodes are less often affected by this pathology.
Joint injuries
Joint pains are provoked by mild traumatic injuries, which cause damage to the ligaments surrounding the joint and bruising of the soft tissues of the joint area. Stronger pain occurs when the meniscus is damaged. The symptom is clearly related in time to a blow, a fall or a difficult movement. Discomfort is usually felt in an affected joint, less often spreading to adjacent areas of the body.
Chronic infectious processes
Possible causes of the feeling of joint pain that occurs without fever or against the background of low temperature are long-term infections. In patients suffering from chronic infectious and inflammatory diseases, joint discomfort becomes a consequence of intoxication of the body or direct harmful effects of microorganisms on joint tissues (usually streptococci, mycoplasma, chlamydia). The appearance or intensification of pain may indicate an exacerbation of chronic tonsillitis, sinusitis, genitourinary infections, adnexitis, pyelonephritis.
Distinctive features of joint pain in common chronic infections that occur with intoxication are moderate severity of joint discomfort, gradual development, periodic intensification and weakening of symptoms. In patients suffering from tuberculosis and hematogenous osteomyelitis, the background for the development of painful sensations is an increase in temperature to subfebrile levels, general malaise - fatigue, weakness, weakness. Without treatment, the condition of patients progressively worsens.
Complications of pharmacotherapy
Taking some medications can be complicated by moderate aches and pains in the small joints of the hands. Unpleasant sensations are not accompanied by redness or deformation of the joints. Patients may complain of muscle pain, fever, skin rash and other manifestations of drug allergies. The anxiety disappears quickly after stopping the drug that provoked it, and it is less likely that special treatment is required for the complications that arise. Pain and mild arthralgia are caused by:
- Antibiotics: penicillin, fluoroquinolones.
- Transvilizing: phenazepam, diazepam, lorazepam etc.
- Contraceptives: combined oral contraceptives (COCs).
Rare causes
- Inflammation of the respiratory system: pneumonia, bronchitis, tracheitis.
- Intestinal pathology: nonspecific ulcerative colitis, Crohn's disease.
- Skin diseases: psoriasis.
- Endocrine disorders: diabetes mellitus, diffuse toxic goiter, hypothyroidism, Itsenko-Cushing disease.
- Autoimmune processes: Hashimoto thyroiditis, vasculitis.
- Fascial damage: necrotizing fasciitis in the convalescent phase.
- Congenital defects of bones and joints.
Survey
To determine why joint and bone pain is felt, it is necessary to consult a therapist or family doctor, who will make an initial diagnosis and prescribe examinations by specialized specialists. Taking into account the nature of the unpleasant sensations, the speed of their appearance and accompanying symptoms, the following is recommended to determine the cause of the disorder:
- Laboratory blood test. An evaluation of the number of leukocytes and the level of ESR is required to exclude infections, inflammatory and oncohematological processes. In systemic diseases, it is important to measure the content of total proteins, the ratio of protein fractions in the blood, specific proteins of the acute phase, markers of rheumatoid arthritis and other inflammations. Tests for the concentration of vitamins, electrolytes (especially calcium), and uric acid help diagnose metabolic disorders.
- Bacteriological examination. Bacterial culture is necessary if the pain felt in the joints and throughout the body is likely to be infectious. Urine, feces, sputum and discharge from the urogenital tract are collected for research. To choose an antimicrobial therapy regimen, antibiotic sensitivity is determined. In doubtful cases, microscopy and culture are supplemented with serological reactions (RIF, ELISA, PCR).
- Sonography of the joints. It is usually used for the clear localization of painful sensations and the suspected presence of rheumatic diseases. Ultrasound of the joint allows us to examine its structure, identify cartilage and bone destruction, preclinical inflammatory changes, and study the condition of periarticular soft tissues. The advantages of the method are accessibility, non-invasiveness and high information content.
- X-ray techniques. Changes in the width of the articular space, hardening of the soft tissues, the presence of calcifications, osteophytes and erosions of the articular surfaces are revealed during radiography of the joints. To improve diagnostic efficiency, special techniques are used - arthrography with contrast, pneumoarthrography. In the initial stages of the lesion, tomography (MRI, CT of the joints) is considered more indicative. Bone density can be easily assessed using densitometry.
- Invasive examination techniques. In some cases, to determine the cause of joint pain, a puncture is performed with a biopsy of the cartilage, the inner layer of the synovial membrane and the tophi. Morphological analysis of biopsy specimens and examination of synovial fluid reflect the nature of the pathological processes occurring in the joint. Simultaneous collection of materials with visual examination of the articular cavity is convenient to do during arthroscopy with tissue biopsy.
A less common way to diagnose the cause of joint pain is scintigraphy with the introduction of technetium, which accumulates in the affected tissues. In recent years, there has been a growing interest in joint thermography as a modern non-invasive method for the recognition of inflammatory diseases, tumors and blood circulation disorders in joints and periarticular tissues. If the number of elements formed in a clinical blood test decreases, an extra-articular bone puncture is performed. Patients with joint pain without fever are advised to consult a rheumatologist and an orthopedic traumatologist.

Treatment
Help before diagnosis
For joint pains associated with physical activity, no special treatment is required, a long rest with dosage of loads is enough. Joint discomfort that occurs during pregnancy usually goes away on its own after pregnancy or is corrected by controlling weight and taking vitamin and mineral supplements. Elderly and obese patients are advised to change their lifestyle: adequate physical activity, a diet with an adequate calorie content with a sufficient content of plant foods.
Pain in the bones, joints and muscles, combined with general malaise and fever, increased sensation of pain and withdrawal up to severe pain and the development of constant pain are indications to consult a doctor. To reduce joint discomfort caused by ARVI, it is recommended to rest, drink enough water, rose infusions and dried fruits. Until serious diseases that provoke joint pain are excluded, self-medication with painkillers, long-term unsuccessful application of compresses, lotions, decoctions, etc. are unacceptable.
Conservative therapy
You can get rid of joint pain with the right treatment, aimed at eliminating the cause of the disorder and individual parts of the mechanism of its development. Etiopathogenetic therapy is usually supplemented with symptomatic medications that quickly reduce the severity of nagging pain and pain. The treatment regimen for diseases that occur with joint pain may include:
- Antimicrobial. Basic therapy for infections is based on the prescription of antibiotics to which the pathogen is sensitive. In severe cases, broad-spectrum drugs are used until the sensitivity of the microorganism is determined.
- Nonsteroidal anti-inflammatory drugs. They reduce the production of inflammatory mediators and thereby inhibit inflammatory processes in the joints. By affecting the central pain receptors, they reduce the degree of joint discomfort. It is used in the form of tablets, ointments, gel.
- Corticosteroids. They have a strong anti-inflammatory effect. Hormonal therapy is the basis for the treatment of systemic collagenosis. In severe and resistant forms of the disease, corticosteroid drugs are combined with immunosuppressants to increase the effect.
- Chondroprotectors. They act as a substrate for the synthesis of protein glycans, a sufficient amount of which increases the elasticity of articular cartilage. Nourishes cartilage tissue and restores its damaged structure. Intra-articular administration of drugs is possible.
- Xanthine oxidase inhibitors. It is used as anti-gout medicine. They block the main enzyme necessary for the synthesis of uric acid, thus reducing its concentration in the body and promoting the dissolution of existing urate deposits.
- Vitamin-mineral complexes. It is recommended for the treatment of joint pain caused by metabolic disorders. The most commonly used drugs contain calcium and vitamin D. They are also an element of complex therapy for inflammatory and metabolic diseases.
- Chemotherapeutic agents. They serve as the basis for most treatment regimens for various types of oncohematological pathologies. Depending on the clinical variant and the severity of the neoprocess, they are combined with radiotherapy and surgical intervention.
Physiotherapy
After the exact cause of pain and reduction of acute inflammation, patients, except those suffering from cancer, are prescribed physiotherapy and exercise therapy. Therapy sessions with microwaves and ultrasound, electrophoresis and pulsating currents have a good anti-inflammatory and analgesic effect. In case of chronic pathology, physiotherapeutic treatment is carried out for several months and is supplemented with spa therapy.
































